Virtual reality surgical training has generated a lot of excitement in medical education – but does it actually work? For surgical residents and program directors evaluating new training tools, the central question is whether practicing in VR translates into real-world surgical skill and better outcomes. The evidence to date is very promising: numerous studies, trials, and program experiences have shown that VR training (such as the PrecisionOS platform) can significantly improve surgical performance and knowledge, often matching or even surpassing traditional training methods on key metrics. Below, we answer this question in detail with data and findings from the latest research and experiences.
Täglicher Archiv: expert
PrecisionOS is a virtual reality (VR) surgical training platform that offers an innovative alternative to traditional surgical training methods. Traditional training for surgical residents often relies on observing real surgeries, assisting when possible, practicing on cadavers or simulators, and gradually taking on cases under supervision. In contrast, PrecisionOS provides immersive, hands-on virtual simulations that complement this apprenticeship model. Below, we break down the key differences and advantages of PrecisionOS VR training versus conventional training approaches, with evidence from research and user experiences.
Objective performance data has finally arrived in orthopedic surgery. This article explores how VR simulation, surgical performance analytics, and mobile metrics move training from “I think I’m better” to measurable, data‑driven improvement and proven readiness.
This FractureLab release solves the biggest gap in surgical training: giving residents safe, repeatable practice of high-stakes surgical steps before they ever reach the OR.
PrecisionOS is redefining orthopedic training through personalized, data-driven, and accessible VR-based surgical education. The new Fracture Lab platform helps surgeons build critical skills, gain adaptive feedback, and achieve mastery anywhere in the world—making lifelong surgical learning more equitable and measurable than ever before.
The future of surgical education is immersive and measurable with Virtual Grand Rounds. Learn how residents gain hands-on virtual practice, guided by global experts, aligned with ACGME/ABOS standards.
Virtual Cadaver Lab transforms surgical training by letting residents watch, practice, and perform procedures in immersive VR. Step into a new era of hands-on, accessible surgical education.
Immersive virtual cadaver labs are redefining surgical education—enabling global access to hands-on innovation, active learning, and real-world digital practice for surgeons and trainees.
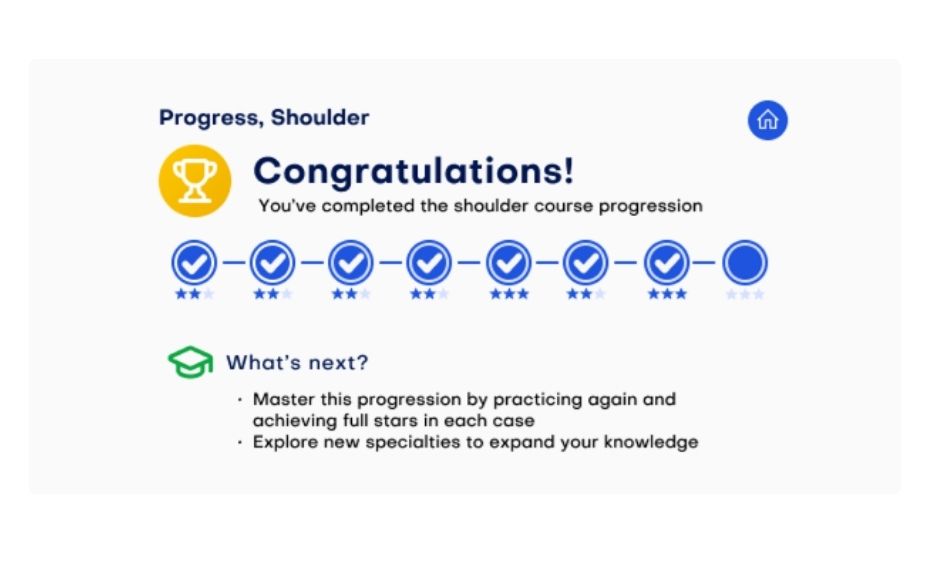
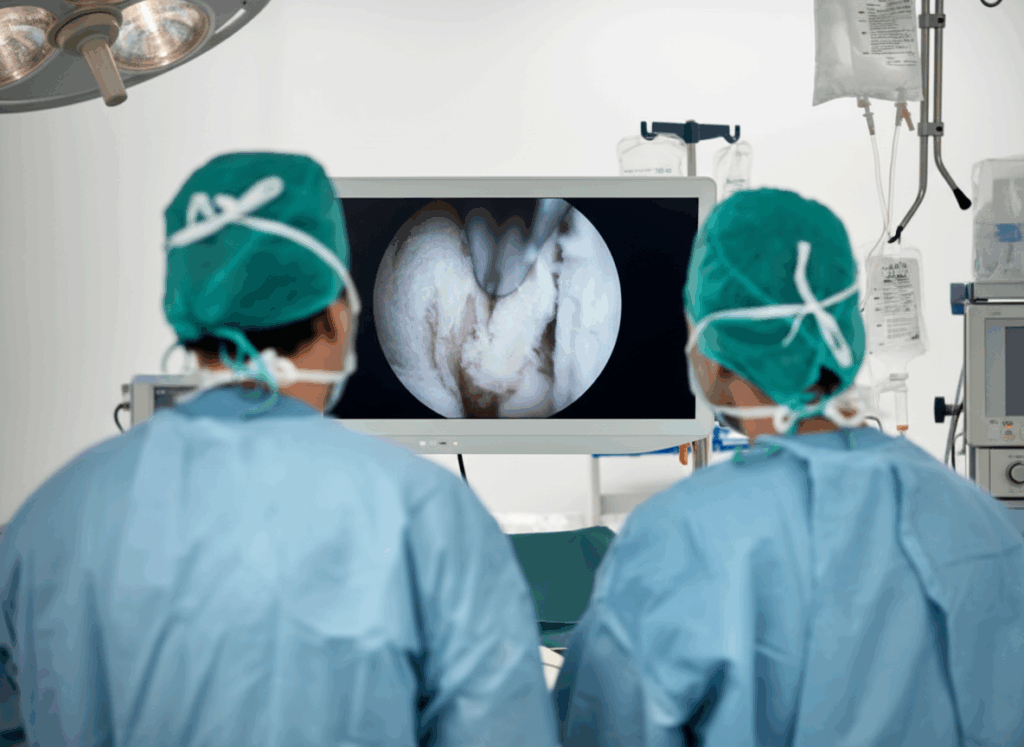
Arthroscopy during residency is one of the steepest learning curves in orthopedic surgery. The technical challenges include mastering the use of angled lenses, interpreting 3D structures on a 2D screen, and handling instruments with precision. Traditional hands-on training with cadaver labs is time-consuming and often limited. Many residents experience slow and unpredictable progress due to intermittent opportunities to practice in the operating room. Virtual reality simulation offers a breakthrough by providing a safe, repeatable learning environment where residents can build skills and confidence efficiently—without the need for costly equipment or cadaver availability.
The IMPACT Initiative unites residency programs, educators, and technology partners to transform orthopedic surgical training. By integrating virtual reality, data-driven insights, and collaboration, IMPACT ensures residents gain structured practice, faculty mentorship is optimized, and patient care outcomes improve.