Introduction
Academic orthopedic surgeons are under increasing pressure to preserve case efficiency while also delivering meaningful operative education. Shrinking OR time, rising patient volumes, and the growing complexity of surgical care have made it harder than ever to balance education with performance. Traditional teaching methods, dependent on real-time instruction, are struggling to keep pace with today’s constraints.
Shifting Strategies
Compounding the difficulty is the fact that residents may only get intermittent, high-stakes opportunities to practice these skills in the OR, making progress slow and unpredictable. Without structured, repetitive practice outside the operating room, even talented trainees can struggle to reach fluency, and teaching becomes a frustrating, inefficient process for both resident and attending.

Teaching arthroscopy is uniquely challenging due to its steep learning curve, reliance on fine motor control, and the need for advanced spatial awareness using a 2D screen to navigate a 3D joint. Unlike open procedures, arthroscopy offers limited tactile feedback and requires the surgeon to interpret depth and orientation entirely through visual cues. For faculty, this means instruction often must be paused mid-case to guide basic camera handling, triangulation, or probe control, disrupting flow, increasing operative time, and sometimes compromising case efficiency.
In this environment, the value of faculty expertise must be protected. Expecting highly specialized surgeons to spend precious OR time teaching foundational skills—like instrument handling, positioning, or basic sequencing—is a misalignment of resources. It’s akin to getting a golf lesson from Tiger Woods, only to spend the hour learning how to hold a club. The OR is the best place to learn, but it should not be the first. By the time residents step into the operating room, they should have already mastered the fundamentals elsewhere—through simulation, deliberate practice, and structured preparation.
Faced with this challenge, faculty surgeons at the West Virginia University School of Medicine, Department of Orthopedic Surgery adopted a new approach. Rather than increasing their teaching load, they shifted their educational strategy by assigning their residents to prepare for surgery independently using the PrecisionOS virtual reality (VR) platform.
This case study explores how WVU integrated PrecisionOS virtual reality simulations into their arthroscopy rotation, allowing residents to develop core technical skills on their own time. In doing so, faculty were able to reduce the instructional burden of basic skills, elevating the quality of intraoperative teaching and maintain full case efficiency, even while granting junior residents more autonomy than ever before.
The WVU Orthopedic Residency Program piloted a six-week initiative focused per resident on the sports rotation with a 12-month continuation for shoulder and knee arthroscopy. Participating residents included the PGY-2s and PGY-5s rotating through sports medicine who were each provided with a Meta Quest 3 headset preloaded with PrecisionOS simulation software. Residents were assigned 10 minutes per week of asynchronous VR training, with simulations aligned to the cases they would be assisting on in the OR.
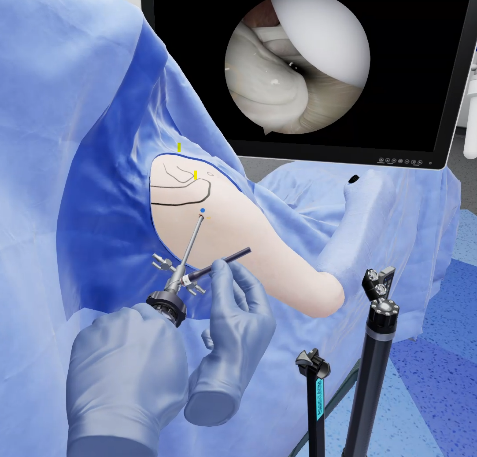
Importantly, faculty were not required to oversee or manage these simulations. Residents logged their training independently, without the need for attending involvement. The goal was simple: allow residents to internalize arthroscopic fundamentals, triangulation, scope control, probe handling, and anchor placement, before stepping into the OR. At the end of each week, the attending received a report which indicated the amount of time each resident practising arthroscopy.
Teaching Transformed: Observed Faculty Outcomes
The most immediate benefit was a reduction in basic instruction. Residents arrived already understanding the procedural flow and required techniques, allowing attendings to skip time-consuming explanations and shift directly into surgical strategy and higher-order decision-making, the critical elements important as an attending surgeon. As Dr. Barry McDonough, Program Director and orthopedic sports medicine attending, observed:
“I didn’t have to pause and explain camera orientation. We could go straight into coaching judgment calls. It made teaching more engaging and beneficial.”
Case preparation time also decreased. Faculty reported fewer interruptions during surgery, less need to micromanage scope navigation, and faster transitions between surgical steps. Perhaps most strikingly, even with PGY-2s performing more advanced parts of the procedure, case durations remained unchanged.
“I let the junior resident do more than I ever had before, and we still finished on time,” said Dr. McDonough. “That tells you how much time VR saves in foundational prep.”
With the burden of mechanical instruction lifted, the nature of teaching in the OR evolved. Attendings described a more collaborative dynamic with residents, where energy could be directed toward interpretation, troubleshooting, and situational awareness, areas traditionally reserved for more senior trainees Which are also critical skills and education around judgment that is valued and critical for patient care.

In short, VR didn’t replace faculty teaching, it elevated it. Residents no longer needed to learn basic skills in the middle of surgery. That meant attendings could engage in true mentorship, not just supervision.
Resident Impact: Enabling Faculty Efficiency
The gains experienced by faculty were driven by observable improvements in resident behaviour. Even PGY-2s demonstrated stronger technical fluency, including smoother scope control, more confident triangulation, and improved tool-handling during diagnostic and debridement phases.
These advances translated into earlier delegation of surgical tasks. Residents began managing more of the procedure with less correction, allowing attendings to permit more independence without concern for safety or efficiency.
From the resident perspective, VR offered a low-stress way to practice before performing. It built confidence, improved orientation, and provided a mental roadmap that translated into better performance during live surgery. With an average session of 7.3 minutes, residents completed 6 virtual reality sessions per month and completed an average of 17 sessions total during the study period.
“I know when I put in 10 minutes in VR, I show up feeling ready,” one PGY-2 explained. “I’m more focused, confident and doing parts of the case I didn’t think I’d touch until next year.”
For academic surgeons tasked with educating residents while meeting institutional performance metrics, this shift is transformative. It allows for earlier trust in junior residents, more meaningful intraoperative teaching, and fewer teaching moments sacrificed for speed.
What emerged from the WVU pilot was a new model for surgical education, one that does not force faculty to choose between teaching and throughput. With asynchronous VR training, faculty did not need to extend hours, add sessions, or increase workload. They simply taught more effectively in the operating room, when it counted.

A Model Without Compromise
What emerged from the WVU pilot was a new model for surgical education, one that does not force faculty to choose between teaching and throughput. With asynchronous VR training, faculty did not need to extend hours, add sessions, or increase workload. They simply taught more effectively in the operating room, when it counted. Most importantly, it protects the sanctity of the OR as an educational space, without slowing it down benefiting the attending surgeon, the resident and ultimately, the patient.
Looking Ahead: Expansion and Future Rotations
Following the success of the arthroscopy pilot, WVU is now expanding the VR training model across additional subspecialties. Rotations in trauma, joint arthroplasty, spine, and upper extremity will all receive tailored simulation curricula aligned with their operative schedules.
Each expansion aims to replicate the same result: prepared residents, empowered faculty, and zero compromise on case flow.
As Dr. McDonough concluded,
“I’m convinced that what used to be a limited experience in our program, arthroscopy training, has now become a highlight. And I didn’t have to lift a finger to make it happen.”
Conclusion: VR as a Faculty-Centric Innovation
Too often, innovation in medical education focuses solely on learners. What this case study makes clear is that faculty gain just as much from virtual reality as residents do. By offloading basic skill acquisition to asynchronous simulation, academic surgeons reclaim their time, elevate their teaching, and trust their residents earlier, all while operating with the same speed and confidence.
To drive greater resident autonomy and surgical readiness, PrecisionOS now enables faculty to teach not just the what but the how—exactly the way they do it. By capturing faculty-specific techniques, preferences, and procedural workflows within the VR platform, residents can practice each step of a surgery precisely as their attending performs it. This eliminates variation and guesswork, ensuring that by the time residents enter the OR, they’re aligned with their faculty’s expectations and methods. The result is a more efficient teaching experience, faster skill acquisition, and a smoother transition to true operative independence. For any program seeking to maximize educational excellence in the operating room in a time-constrained system, PrecisionOS isn’t just a learner tool. It’s become an asset for faculty as well.
About PrecisionOS
PrecisionOS is an award-winning medical software company redefining surgical training through virtual reality. Built by surgeons for surgeons, PrecisionOS empowers healthcare teams around the world with immersive, measurable, and patient-centered learning experiences.
info@precisionostech.com
www.precisionostech.com


